BJS Academy>Cutting edge blog>Guest post: The effe...
Guest post: The effects of COVID-19 on surgeons and patients
Gianluca Pellino (@GianlucaPellino) and Antonino Spinelli (@AntoninoSpin) are surgeons from Italy.
18 March 2020
Guest Blog General
Related articles

Invited Commentary: Associations between adverse outcomes for surgical admissions and nurse understaffing – a longitudinal study
Petter Frühling, MD, PhD,1 and Patricia Tejedor, MD, PhD2
1. Hepatobiliary and Pancreatic Unit, Department of Surgery, Department of Surgical Sciences, Uppsala University Hospital, Sweden.
2. University Hospital Gregorio Marañón, Colorectal Surgery Unit, Madrid, Spain
In a recent study published in BJS, Meredith1 and co-authors present their findings of the detrimental effects of nurse understaffing and adverse events for surgical patients. This, as the authors highlight, is a critical yet often overlooked problem that extends far beyond the National Health Service (NHS) in England. Although the paper’s conclusion that ‘understaffing’ is ‘associated with increased risks of a range of adverse events’ may appear obvious, the significance of the findings relies on its universal character – that it is a global problem that requires urgent attention.
The World Health Organization (WHO) has de facto identified a global shortage of healthcare workers, particularly nurses and midwives, who represent more than 50% of the current shortfall. While the shortage of doctors may be manageable, the understaffing of nurses poses a severe threat to health outcomes. In a large observational study, that included nine European countries and data from more than 420 000 patients, published in Lancet in 2014, it was noted that each increase of one patient per nurse was associated with a 7% increase in the likelihood of a surgical patient dying within 30 days of admission2.
Two recent reports from the International Council of Nurses (ICN) further emphasise the detrimental effects of nurse understaffing on patient outcomes, and urge readers to view this as a matter of global urgency. In Sustain and Retain in 2022 and Beyond3 the authors project the need to replace up to 13 million nurses globally in the coming years, reflecting alarming rates of nurse attrition driven by stress, burnout, absenteeism, and industrial action. The ICN’s 2023 follow-up report, Recover to Rebuild – Investing in the Nursing Workforce for Health System Effectiveness , calls for a coordinated global effort to establish a sustainable nursing workforce through a long-term, ten-year plan.
Surgical research in Plain English
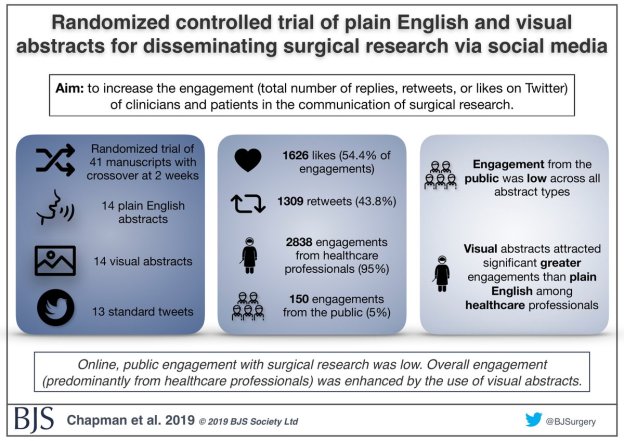
Randomized controlled trial of plain English and visual abstracts for disseminating surgical research via social media
BJS started with the aim of of being a medium through which surgeons “can make our voice intelligibly heard”, according to Sir Rickman Godlee, President of the Royal College of Surgeons of England in 1913.
The aim of a recently published paper in BJS was to increase the engagement (defined compositely as the total number of replies, retweets, or likes on Twitter) of clinicians and patients in the communication of surgical research – part of the core values of BJS.

Prioritising Surgical Treatment in Coronavirus Pandemic “Salford Score”
Prof Gordon Carlson CBE FRCS
Background
In light of the need to assess priorities of surgical treatment in a resource-limited environment, NHS England have set out clinical priorities for cancer surgery. However, these priorities do not take into account the vulnerability of the patient to excess morbidity and mortality in the event of Covid-19 infection. It seems evident that, particularly when undertaking elective surgery, the vulnerability of a patient to Covid-19 related morbidity and mortality might be equally important to considerations of the timing of surgery as the underlying disease for which surgery is proposed.
The resource allocation system currently in use at Salford Royal NHS Foundation Trust (which has since been adopted throughout other hospitals at Northern care Alliance) takes both of these factors into account, by producing a score based upon the need to prioritise treatment on purely disease related grounds and also the vulnerability of the patient to Covid-19. The aim is to generate a score which can be used to determine the overall surgical treatment priority of a group of patients, possibly from different surgical subspecialties, when surgical resources have become limited as a result of the Covid-19 pandemic. The score allows different groups of surgeons and hospital management to objectively determine how temporarily limited resources might be allocated. It is meant to help guide collective discussions, not to be a rigid indicator of those patients for whom surgical treatment should be deferred, and it should be used to support, not to replace MDT discussions.
Copied!
Connect

Copyright © 2026 River Valley Technologies Limited. All rights reserved.



.png)





.jpg)



