Cutting edge blog
This section is designed to add value to the articles published in BJS and BJS Open.
If you wish to send a written (or even recorded) comment on one of the published articles, please send it to katie@bjsacademy.com.
If you wish to respond more immediately, please use social media directly by tagging @BJSurgery, @BjsOpen or @BJSAcademy
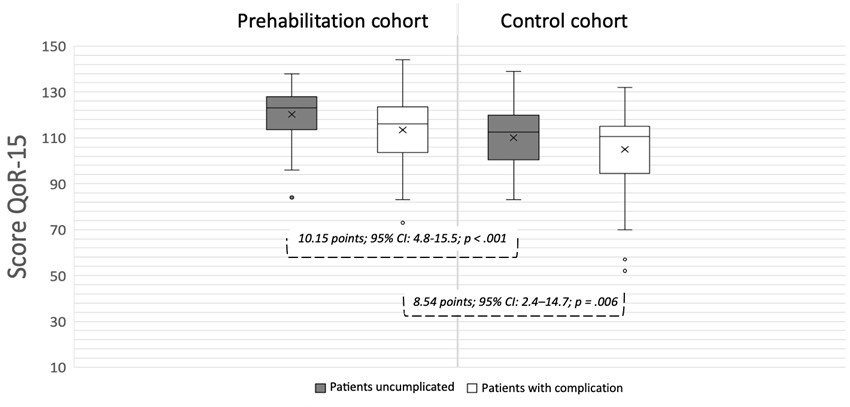
Multimodal prehabilitation: beyond physical preparation
Fernando Dana

Comment on: Endoscopic and surgical treatment options for gastroparesis: systematic review and network meta-analysis.
Martin Storr, Thomas Frieling, Jutta Keller, Felix Gundling, Robert Patejdl

Author response: Endoscopic and surgical treatment options for gastroparesis: systematic review and network metaanalysis
Daniel Eckhardt, Moustafa Elshafei, Katja Fechner, Markus K. Diener, Felix J. Hüttner

Comment on: Breast satisfaction and health-related quality of life following total mastectomy, breast-conserving surgery, or immediate breast reconstruction in Japanese patients with breast cancer: multicentre cross-sectional controlled study (Reborn)
Janhavi Venkataraman, Kefah Mokbel

Author response: Decreasing aortic diameter and decreasing prevalence of infrarenal aortic aneurysms in a population-based screening programme
Antti Siika, Rebecka Hultgren

Comment on: Decreasing aortic diameter and decreasing prevalence of infrarenal aortic aneurysms in a population-based screening programme
Antonio Manenti, Gianluca Pagnoni, Aurora Vicenzi, Francesca Coppi

Pancreatic Cancer Awareness 2025

Science and art of decision-making in surgery
Susan J Moug

An introduction: 'Presidents Under the Knife' blog series
Per-Olof Hasselgren, MD, PhD

Comment on: Quality of life in patients with permanent hypoparathyroidism after thyroidectomy for benign thyroid disease: population-based study with long-term follow-up
Zhaoyu Peng, Yongjin Chen, Zou Meng, Wenjiang Wu

Author response: Quality of life in patients with permanent hypoparathyroidism after thyroidectomy for benign thyroid disease: population-based study with long-term follow-up
Matilda Annebäck, Sofia Wachtmeister, Jakob Hedberg, Peter Stålberg, Olov Norlén

Fascial closure in IPOM repair: the case for long-term follow-up and clinical transparency
Ming Wang

Author response: Fascial closure in IPOM repair: the case for long-term follow-up and clinical transparency
Mikael Lindmark, Jael Tall, Bahman Darkahi, Johanna Österberg, Karin Strigård, Anders Thorell

Assessing reinforced tension line sutures for hernia prevention: methodological considerations from the Rein4CeTo1 trial
Anshika Upasani

Comment on: Management of bilioenteric anastomosis leakage after major liver resection
Christian Sturesson, Melroy D’Souza, Cecilia Strömberg, Ernesto Sparrelid, Stefan Gilg
Surgery and the future of breast cancer care: breast cancer awareness month 2025
Matthew Lee PhD FRCS

Team design as innovation in perioperative care: the case of HPB anesthesiology
Julie Hallet, MD MSC, Naheed Jivraj, MD MSc

Author response: Missing the split? Reconsidering the scope of biliary complications in the classification proposed at the BileducTx meeting
Hannah Esser, Iris de Jong, Floris M Roos, Robert J Porte, Stefan Schneeberger

Comment on: Ultra-low dose superparamagnetic iron oxide nanoparticle injection for sentinel lymph node detection in breast cancer: prospective cohort study
Lielong Yang, Yuzhou Zhu

Author response: Ultra-low dose superparamagnetic iron oxide nanoparticle injection for sentinel lymph node detection in breast cancer: prospective cohort study
Fredrik Wärnberg, Andreas Karakatsanis, Roger Olofsson Bagge

Reproductive outcomes after ileo-pouch anal anastomosis: clarifications and the importance of fertility counselling
Anders Mark-Christensen, Kirstine Kirkegaard, Mette Julsgaard

Birth rates and fertility are not the same
Eugenia Shmidt, Zoë S. Gottlieb, Marla C. Dubinsky

Comment on: Oncological, surgical, and cosmetic outcomes of endoscopic versus conventional nipple-sparing mastectomy: a meta-analysis
Kefah Mokbel, MBBS, MS, FRCS

Endoscopic mastectomy meta-analysis: commentary
Ayla Carroll, Carlos Robles, Hung-Wen Lai, Lidia Blay, Piotr Pluta, Gauthier Rathat, Guillermo Peralta, Rami Younan, Giada Pozzi, Daniel Martinez Campo, Robert Milligan, Glenn Vergauwen, Paolo Carcoforo, Antonio Toesca








.jpg)




